Clinical presentation of pain symptoms in patients with Bertolotti’s Syndrome is not always straightforward. Therefore, the diagnosis of Bertolotti's Syndrome is a multi-step process that requires a critical review of patient history, thorough physical imaging, precise imaging, and often, physiological confirmation with diagnostic injections.
Diagnostic protocol for Bertolotti’s Syndrome
Click images to proceed to each section
Age of onset - Patients with Bertolotti’s Syndrome tend to present with chronic lower back pain may that started early in life. Some patients have been diagnosed as early as mid-to-late teens (Ali & Enchev, 2023). A recent retrospective cohort study of 150 individuals by Jenkins et al showed that the average age of the cohort was 49 years old (Jenkins, O’Donnell, et al., 2023). Given the rarity of the condition, it is possible that patients get diagnosed with Bertolotti’s Syndrome much later in life.
Type of pain – Individuals with Bertolotti’s Syndrome may present with a myriad symptoms. This variety arises from several factors including the different types of LSTV, the presence of comorbidities (e.g., disc herniation), and other congenital conditions (hEDS). Despite this, there are some symptoms that are largely maintained across most individuals. These include pain symptoms considered to be typically mechanical in nature, i.e., aggravated by movement. The main aggravators of symptoms tend to be lumbar flexion and rotation. Some patients also experience discomfort from prolonged sitting and certain sleeping positions.
Physical exam can reveal localized tenderness around the posterior superior iliac spine (PSIS), the SI joint, and the paraspinal muscles (Adams et al., 2018). Furthermore, individuals present with limited lumbar range of motion as well as positive tests on the FABER and Gaenslen tests (Adams et al., 2018; Alonzo et al., 2018). Given the non-specificity of a physical exam in diagnosing Bertolotti’s Syndrome, it is important that it is coupled with the appropriate radiological imaging and diagnostic injections.
Definition:
FABER test – this is a clinical pain provocation test to help diagnosed pathologies of the lumbar spine, sacrum, and hip. The test involves moving the patient through Flexion, Abduction, and External Rotation (FABER).
Gaenslen test – this is used to assess pain originating from lumbar spine or SI joint. The test is conducted with patient in supine position with legs on the edge of the treatment table.
NOTE: neither of these tests are non-specific and do not provide definitive insight on whether a patient has Bertolotti’s Syndrome. They merely indicate the presence of lumbosacral or hip pathology.
Diagnostic imaging is a critical component in the diagnostic protocol for Bertolotti’s Syndrome. It is used to identify the presence, and type, of LSTV. Furthermore, it helps identify other potential pathologies that could be contributing to the patient’s symptoms. The imaging modalities utilized are as follows:
X-ray – Clear visualization of the lumbosacral region for the purpose of identifying LSTV requires a combination of three imaging views and three positional postures: anteroposterior (AP), lateral, and Ferguson view (Konin & Walz, 2010).
Recommended X-ray views for identifying LSTV
AP (Anteroposterior) View
Taken from the front of the patient, with the X-ray beam directed straight through the abdomen to the back.
Used to assess the alignment and width of the transverse processes and their relation to the sacrum.
Image is taken while patient maintains a neutral posture (standing upright with a natural spinal posture).
Lateral View
Taken from the side of the patient, with the shoulder positioned closest to the X-ray detector.
Helps visualize the disc spaces, vertebral body alignment, and the relationship between L5 and S1 from a sagittal (side) perspective.
Images need to be taken at neutral , flexion (bending forward) and extension (bending backward) positions.
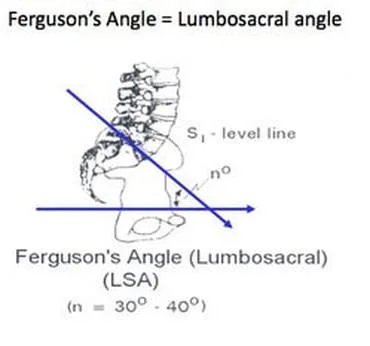
Ferguson View
Involves angling the X-ray beam cranially (upward) at 30–40 degrees while the patient remains in the AP position.
Enhances visualization of the lumbosacral junction, specifically the transverse processes of L5, and their articulation or fusion with the sacrum.
Image is taken while patient maintains a neutral posture.
Magnetic Resonance Imaging (MRI) – MRI goes beyond identifying the presence of LSTV. It helps to clearly evaluate soft tissue in the lumbosacral region. It helps identify any comorbidities that could be the source of the patient’s pain such as disc herniation, annular tear, facet joint arthrosis, and nerve root compression (Alonzo et al., 2018).
Computed Tomography (CT) scan – This is considered to be the best method to visualize LSTV. However, it is not the preferred imaging technique for assessing the presence of LSTV since it exposes patients to radiation (Konin & Walz, 2010). Furthermore, CT images are used develop a 3D model of the lumbosacral region which can, in turn, aid in the devising appropriate surgical approach. In certain cases, SPECT/CT scans are used to locate the site of pain. This technique uses a radioactive tracer that localizes to sites of osteoblastic activity which localizes to the sites of arthrosis formed due to the pseudo-articulation formed by LSTV (Riyami et al., 2017). It is important to note that patients with Bertolotti’s Syndrome may not always have positive signal on SPECT/CT scan. A negative SPECT.CT scan results does not rule out LSTV as the pain generator. This must be confirmed using diagnostic injection.
An important outcome from diagnostic imaging is that we can accurately determine the LSTV classification. The modern classification of LSTV anatomy was first introduced by Antonio Castellvi to characterize the different types of transitional anatomy observed in patients (Castellvi et al., 1984). However, this classification has several limitations. First, the classification was developed to identify lumbosacral disc herniations in patients. Second, it fails to consider contact of the enlarged transverse process to the iliac crest. These limitations were addressed by Dr. Arthur Jenkins and his team in their revised LSTV classification dubbed Jenkins classification (Jenkins, O’Donnell, et al., 2023).
The presence of LSTV does no necessary mean that it is the pain generator. The final and most critical step in the diagnostic protocol for Bertolotti’s Syndrome is the fluoroscopy-guided diagnostic injection at the site of pseudo-articulation with just a local anesthetic (e.g., lidocaine or bupivacaine). The injection is considered to be positive if the patient experiences more than 80% reduction in their pain symptoms (Jain et al., 2013; Jenkins et al., 2023). A negative result after the injection indicates that the LSTV is not the pain generator.